Deck the halls with Ty- le -nol -y
fa la la
la la, la
la la la
‘Tis the season to be snotty,
fa la la la la la
la la la
Don we now our dirty jammies,
fa la la
la la la
la la la…

We’ve been hit hard by viral upper respiratory tract infections. Every preschool and school-age child is snotty-nosed and coughing. Every college student is sick. Fevers and body aches abound. Folks are sick for weeks on end with one viral infection after another.
As a retired board-certified emergency physician who now works in college health, I wanted to discuss when people need to be concerned about their cough, stuffy head, and fever, when they should see a medical care provider, and when they need to snuggle in bed and recover from their viral upper respiratory tract infection for however long it takes.
Upper respiratory infections present many different symptoms and require different care depending on the cause of the infection. Some may necessitate a trip to the Emergency Department, while some require an office visit with your primary care provider, and yet others are safe to stay home with. I’ve divided a list of symptoms into those that require emergency treatment and those that require a check-in with your doctor.
Regarding upper respiratory tract infections, please go to the Emergency Department immediately if you experience any of the following symptoms:
- Trouble breathing. You may feel like you are not getting enough air or can’t catch your breath or you may have a rapid respiratory rate, or you may have to work hard to be able to breathe
- Bluish or purplish discoloration of your skin or lips, or if you are extremely pale
- A pulse oximeter reading below 92%
- Significant chest pain with your upper respiratory infection
- Being unable to drink or keep down fluids and having no urine output for more than 6 hours
- Passing out or nearly passing out with standing
- Being unable to swallow saliva and actually drooling due to sore throat (this is different from pain during swallowing)
- Being unable to open your mouth widely and having a sore throat
- Being confused or delirious even when the fever is down
- Having an isolated headache with a stiff neck and fever with or without a rash.
The following are examples of when you can likely get medical care from your primary care provider for your upper respiratory tract infection:
- Wheezing due to your upper respiratory infection, but not feeling short of breath
- A pulse oximeter that is reading below 95% but above 92%
- A prolonged high fever without another obvious cause (by prolonged, I mean more than 4-5 days in a row)
- A SINGLE SINUS (on one side only) that is painful, with one-sided green nasal discharge, with or without fever
- Being unable to drink or keep down fluids and having low urine output or dark urine but still urinating at least every 4-6 hours
Now that you have a basic idea of what symptoms require which kind of care, I would like to talk about upper respiratory tract infections in general and things you can do to prevent these sorts of infections. Then, I will get into some specific types of upper respiratory infections that doctors see regularly, and discuss some inexpensive medications and equipment you can have around your house to help you get through the season of sickness.
Please note that a cough, even one that produces phlegm, may linger for several weeks beyond the acute illness. The duration that you have a nagging cough after an upper respiratory tract infection does not indicate anything about the severity of the infection or your need for antibiotics.
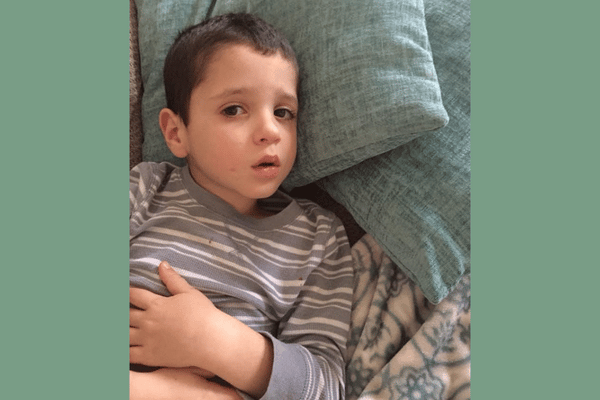
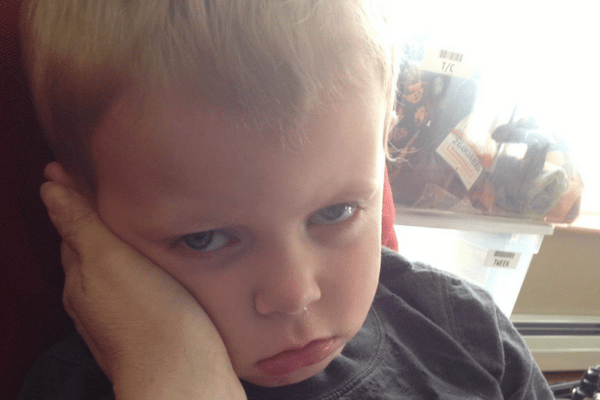
 Does it seem like your child is sick all the time? They probably are!
Does it seem like your child is sick all the time? They probably are!
In an average year, an AVERAGE preschool or school-age child (the same holds true for college students especially if they are living in dorms) gets 8-12 upper respiratory tract infections, each lasting 1-2 weeks. These are concentrated usually in the fall and winter months.
Cold and flu season is the seven months between November and April. You can expect 8-12 upper respiratory infections in seven months. That is 1-1.5 upper respiratory tract infections each month, each lasting up to 2 weeks.
That means that ON AVERAGE, kids (and college students) are sick AT LEAST half the winter with viral upper respiratory tract infections.
Plan on increasing the number of illnesses and the duration of each illness if the child/student lives with a smoker or smokes themselves (this includes marijuana, vape, etc). Healthy nonsmoking adults without exposure to preschool or school-age children get sick a bit less than average.
This is frustrating news, but knowing what normal is can help quell a lot of the worry about yourself or your child being sick all winter.
The thing is, this upcoming winter is also NOT AN AVERAGE WINTER. The COVID-19 pandemic has thrown seasonal virus schedules off worldwide, this is the first winter where most of the population is not masking, children have not had the opportunity to build immunity to the normal winter viruses in the last couple of years, and pretty much all hell is breaking loose everywhere in terms of viral upper respiratory tract transmission right now. Because of this, people are likely to get MORE than the average number of viral upper respiratory infections this year.
So, what can you do to protect yourself and your children from these raging viral illnesses?
Wear a mask in crowded or indoor spaces
I know, I know, you are sick of masks. I am too. But, it is the most effective way to keep from getting sick with an upper respiratory tract infection. When there was universal masking, there was no flu season in either hemisphere. No one got sick. I love my masks because I have not gotten even vaguely sick in 3 years.
Get VACCINATED and boosted if applicable
Both for COVID AND FLU. Hopefully, there will be an RSV vaccine someday soon. Flu is circulating right now so get your flu vaccine NOW. Vermonters can attend free public vaccination clinics for both COVID and flu vaccines.
Wash your hands
Get plenty of rest, good food, and fluids to give your body the best chance to fight off infections
Stop smoking EVERYTHING
If you can’t do it for yourself, do it for your kids. Your smoking is making them (and you) get more upper respiratory infections and is making it harder to get over upper respiratory infections when they (you) are sick. Even if you only smoke outside, the smoke particles remain in your clothing and have the same effect on your children
Finally, if you feel sick, don’t socialize!
It doesn’t matter what you have. If you don’t feel well, stay home. If you MUST go out, wear a mask to prevent spread.
Now let’s talk about some specific illnesses that you might have heard of that can cause upper respiratory tract infections.
COVID-19
COVID is still circulating! It can cause symptoms of upper respiratory tract infection or isolated gastrointestinal symptoms like diarrhea, vomiting, and nausea. If you are sick, test for COVID on the first day of your illness and at least every other day until about day six. It is not sufficient to only test once early in the illness and assume you do not have COVID. If you are at high risk for COVID because of age, vaccination status, underlying disease, or medications, contact your provider as soon as possible to discuss treatment options if you do test positive.
For everyone else, care for someone who tests positive for COVID focuses on addressing the symptoms and staying isolated to prevent spread. Symptoms of fatigue, mucus, cough, sinus congestion, brain fog, dizziness, poor exercise tolerance, depression, and/or anxiety may linger for several months beyond the acute illness.
(All Vermonters with insurance of any kind can get up to 8 free at-home COVID tests per month/person billed through insurance with no out-of-pocket expense- keep them on hand!)
Flu
When we talk about flu, we mean Influenza A and B. These viruses make people suddenly miserable with fever and body aches as well as headache, sore throat, stuffy head, runny nose, cough, and possibly nausea, vomiting, and diarrhea. People are usually sick IN BED for 7-10 days. They are miserable. There is a medication available to treat flu, but unless you are at high risk for severe complications from flu (pregnant, asthma, elderly, chronic disease, etc) the medicine is not all that effective in helping you feel better sooner (it offers about 8-12 hrs decrease in symptom duration out of a 10-day illness if taken early in the course of the illness) and it has potential side effects of nausea, vomiting, headache, and fatigue. Most healthy non-pregnant people with flu opt for symptomatic care with medications to help control the bothersome symptoms.
Flu-like Illnesses
These viral infections present with all of the symptoms of flu but show negative for flu during testing. They usually have a much shorter duration of fever, body aches, and being sick in bed (3-5 days rather than 7-10.)
 Fever
Fever
Healthcare providers count a fever as any temperature over 100.4 F. It doesn’t matter if you usually run low, 99 is still not counted as a fever. Fever, in and of itself, is not dangerous or even harmful (unless you are under 60 days old, or immunocompromised in which case you need to go to the emergency department) In fact, our immune systems work better at a higher temperature, which is why our body generates a fever when we are sick.
Fever is a sign of infection and is common with viral upper respiratory tract infections or bacterial infections like pneumonia (which requires antibiotic treatment.) Although fever is not dangerous, it feels MISERABLE, and, in some young children, can cause febrile seizures which are terrifying for parents (although also not dangerous). I treat fever if patients are uncomfortable, or in a child with a history of febrile seizures. I don’t treat fever just to treat it.
Common Cold
People with the common cold usually have some combination of stuffy head, runny nose, sore throat, cough, fatigue, and pink eye- without fever and body aches. People generally feel well enough to be out and about. Symptoms of a cold, including cough and stuffy head, can last several weeks beyond the acute illness, and symptoms tend to migrate around the body from one spot to another (sore throat, then head cold, then cough, or something similar, etc.)
Bronchitis
Bronchitis means you have an infection in your bronchi. The bronchi are the large airway passages leading to the lungs. This is diagnosed by listening to the lungs. Treatment for bronchitis takes into consideration medical history. In young healthy people, bronchitis is largely VIRAL and is not treated with antibiotics. I see patients all the time who have a history of bronchitis and say they always get better with antibiotics.
This is because they would get better no matter what, with time- with or without medicine.
Viruses resolve on their own, in their own sweet time. They make people feel terrible while they are around, but will not respond to antibiotic treatment. (If you have COPD, emphysema, or other chronic lung disease, antibiotics may be needed as the infection may not resolve without them- see your provider.) In healthy people, bronchitis is a subset of upper respiratory infections and can be treated the same way.
Bronchitis is different from pneumonia.
Pneumonia
Pneumonia is an infection of the lungs that can be either viral or bacterial (or rarely fungal) and often requires antibiotics. Pneumonia usually presents in patients as a cough associated with fever, chest pain, shortness of breath, shaking chills, and headache. It is NOT associated with a sore throat, stuffy nose or head, or other cold symptoms. Diagnosis is made by chest x-ray or by abnormal lung sounds consistent with pneumonia in a patient with concerning symptoms.
Sinusitis
Viral Sinusitis
This is another case where I see people thinking they need antibiotics when, in fact, they have a viral infection causing congestion of the sinuses. When asked what symptoms patients have that make them think they need antibiotics, I most commonly hear about some combination of green snot from both nostrils and pressure in either all four sinus cavities (there are two frontal and two maxillary) or just the two maxillary or just the two frontal sinus cavities.

Green snot from both nostrils and even pressure in two or four of the sinus cavities is most commonly viral and will not resolve from antibiotics any sooner than if antibiotics were not given. Symptoms of congestion and green snot can last for several weeks and still be viral.
Bacterial Sinusitis
Bacterial sinusitis usually impacts one of the SINUSES on ONE side of the face. That one side will be fully congested, painful, hurt more when you bend over or tap on it, and give facial or dental pain on that side. It will also be associated with green snot from JUST THAT SIDE (the other side is clear). It is often also associated with fever. Bacterial sinusitis can occur after viral sinus infection and congestion but generally comes with the sudden worsening of just that one sinus rather than lingering green boogers and pressure throughout the entire face and head.
Bacterial sinusitis may require antibiotic treatment, so if you have these symptoms, please see your medical care provider.
Ear Infections
Once again, most ear infections are viral and do not need to be treated with antibiotics. Doctors in the US recognized that in Europe and other parts of the world, most ear infections had not been treated with antibiotics for over two decades, yet these countries had the same infection outcomes we did while prescribing antibiotics for ear infections. This is hard to hear for many parents who are accustomed to getting antibiotics for their child’s ear infection and are resistant to leaving the office without a prescription. Most pediatricians request that patients wait two days before starting antibiotics for many ear infections because ear pain often resolves without antibiotic treatment. During those two days, treating with pain control and trying to clear the congestion as described below is advised.
Pink Eye
Is the white of your eye red and irritated, with the lids glued closed by goop in the morning and watery/gritty during the day? This is pink eye and is largely viral especially when there have been symptoms of an upper respiratory infection. Viral pink eye is very contagious and commonly spreads from one eye to the other.
Antibiotic drops DO NOTHING to help viral pink eye. I have no idea why schools and preschools allow kids to come back to school when they have been treated with antibiotic eye drops since this is a viral infection. Hand washing, changing pillowcases, not touching the face, throwing away eye makeup, and discontinuing contact lenses is the best treatment. Symptoms will resolve in 3-5 days (but often not before spreading to the other eye and to other people in the household or school).
Laryngitis
Laryngitis means that your larynx (voice box) becomes inflamed and you lose your voice. If you have no voice with your other upper respiratory tract infection symptoms, it is almost definitely viral.
Isolated Sore Throat
A few words about a sore throat. I see lots of people with sore throats related to a viral infection that includes symptoms of cough and stuffy head, runny nose, and swollen glands. When these symptoms are present with a sore throat, this is almost never strep throat, especially if there is an associated cough. If the sore throat is the ONLY complaint or is present with fever, headache, and fatigue, but without the other cold symptoms, the likelihood of strep throat is higher.
Strep throat is tested for by either a rapid strep test which is available immediately or with a throat culture which takes a couple of days to produce results. We treat strep throat with antibiotics, not to change the time course or severity of the sore throat symptoms, but to prevent long-term complications of rheumatic fever and rheumatic heart disease related to strep infection, and to decrease transmission.
Mononucleosis
Mononucleosis, or mono, Is caused by the Epstein-Barr virus. Since this is a virus, the only treatment is symptomatic care. It does not respond to antibiotics. We expect people with mono to be sick for longer than people with most other infections and want them to avoid contact sports as mono can cause the spleen to enlarge.
In general, if multiple people in your household (or friend group or dorm) are sick with a similar variety of symptoms (runny nose, cough, sore throat, stuffy head, etc) you can put your money on the fact that you have a virus circulating. If multiple people have sore throat symptoms only, testing for strep or mono is reasonable.
Respiratory Syncytial Virus, or RSV
This virus is making the headlines these days for filling pediatric hospitals and emergency departments with very sick children. RSV is a common virus that most people experience as a common cold. However, it can make some very young children, especially those who are premature or under one month old, or the elderly, very sick with viral pneumonia or something called bronchiolitis (different than bronchitis).
Routine testing for RSV will be done if a patient is admitted to the hospital or is in the Emergency Department with upper respiratory tract infection symptoms and is high risk, but it does not need to be done if the patient is doing fine at home with their cold symptoms. It will not change management, which is centered around alleviating symptoms and preventing spread.
 Why do we care about giving antibiotics to people with a viral illness, and more importantly, why should you care if you are getting antibiotics unnecessarily?
Why do we care about giving antibiotics to people with a viral illness, and more importantly, why should you care if you are getting antibiotics unnecessarily?
Antibiotics are one of the 20th century’s most important medical discoveries. They are one of the few things we can do for people that can truly prevent serious illness and death. When you need antibiotics, you NEED THEM. Having said that, when you don’t need antibiotics, they cause more harm than good when taken.
The problems with unnecessary antibiotic use include:
- Serious, life-threatening allergic reactions
- Minor allergic reactions
- Diarrhea and gut flora disruptions (with all sorts of implications for your overall health and well-being)
- Yeast infections of the mouth and vagina
- The creation of antibiotic resistance in the individual and world at large
In addition to these direct effects of unnecessary antibiotics, there are also indirect effects. These include:
- The time, energy, and money you spend going to your provider unnecessarily to obtain a prescription
- The strain these unnecessary visits put on an already taxed healthcare system
- Exposing you or your child to people with other viral illnesses in the waiting room, and exposing them to you
So if, after reading this, you feel like you have a viral illness and are not experiencing any worrisome symptoms, you can save yourself lots of hassle and stay home drinking hot lemon water with honey.
Supplies and treatments every house should have to deal with upper respiratory tract infections
Pulse oximeter

Thermometer
This is less important than a pulse oximeter unless you have an infant under 60 days old or are immunocompromised.
Neti Pot
This can be used to perform a sinus rinse, and combined with a decongestant, is the best treatment for sinus congestion. Do a sinus rinse twice a day while taking decongestants (if tolerated.) Do not smoke anything for the most rapid resolution of your sinus symptoms. Use only distilled water for your Neti pot. You can buy a Neti pot at any pharmacy for $10-$20.
Acetaminophen (Tylenol)
This can be used for pain or body aches and fever. DO NOT TAKE more than directed. It is dangerous or fatal in overdose.
Ibuprofen (Advil, or Motrin) or Naprosyn (Aleve)
These are non-steroidal anti-inflammatory drugs (NSAIDs) and can be used for pain, inflammation, and fever.
Acetaminophen and ibuprofen (or Naprosyn, if preferred) can each be taken following the bottle instructions and can also be taken TOGETHER if needed for fever and pain control.
If taking a combination cold remedy like Nyquil or Mucinex, DO NOT ALSO TAKE ACETAMINOPHEN, or other acetaminophen-containing medications, since these products likely contain it already. There are some Mucinex products that do not contain acetaminophen, but check the label). You can, however, take the combination cold medicines along with NSAID medications.
Cough suppressant with dextromethorphan (anything labeled DM)
This can be used for an annoying cough that is keeping you awake at night or disrupting you in class. (Not appropriate or effective for young children- see bottle for age restrictions- usually not recommended to be given to children under age 6.)
Expectorant cough medicine with guaifenesin
This is used to loosen mucus and make you cough MORE (if that’s what you want/need.)
This is used for a cough that feels like you have gunk in your chest or throat that you need help coughing out. Remember, you may cough MORE with this. (Not appropriate for young children. See bottle for age restrictions, usually not recommended to be given to children under age 6.)
Decongestant (pseudoephedrine, if you can tolerate it) for sinus congestion.
(Not appropriate for young children. See bottle for age restrictions. Usually not advised for children under age 12.)
Combination cold medicines like Nyquil/ Dayquil contain acetaminophen, cough suppressant, and decongestant while Mucinex has many formulations with a variety of ingredients but all contain guaifenesin and some contain acetaminophen and dextromethorphan as well. Please check what you are buying and do not take more than recommended. Do not take acetaminophen-containing multi-symptom products in combination with acetaminophen.
Warm salt water gargles
This really helps! Not only is it soothing, but warm water also draws blood to an area (that’s why your skin gets red in a hot shower- increased blood flow to the skin) and blood carries your white blood cells which help fight infection. Gargling warm water helps to assemble infection-fighting white blood cells exactly where they are needed. High salt concentrations help kill viruses and bacteria. Do warm salt water gargles at least twice a day to help your sore throat.
Honey
For children, honey is as effective as cough medicine, and without the risks! It also works in older children and adults. It can be taken alone or mixed in a warm fluid. Honey is also helpful for sore throats. Never give honey to children under 1 year.
Albuterol
Sometimes people wheeze when they have upper respiratory infections, and in these people, albuterol can be helpful. If you or your child have wheezing, you should see your provider and ask about this treatment.
Liquids
When you are sick, your fluid needs are higher than usual. Drink non-alcoholic, caffeine-free liquids until your urine is clear. Good hydration is likely as effective as guaifenesin for loosening mucus. Chicken broth, herbal tea, juice, ginger ale, popsicles, watermelon, and cucumbers are all very hydrating.
 Other helpful techniques for managing upper respiratory tract infections
Other helpful techniques for managing upper respiratory tract infections
Since cough medications and decongestants are not recommended for young children due to potential side effects of excessive sleepiness or agitation, relying on acetaminophen, ibuprofen, honey, warm salt water gargles (if the child is old enough to reliably spit out the salt water- if not, just warm water gargles or warm drinks), and saline nasal rinse or saline nose suctioning, as well as spending time near a steamy shower are your major weapons against the discomfort of viral upper respiratory tract infections.
It can be helpful for both children and adults to sleep propped up in bed a bit rather than lying flat and to open the window in the bedroom for sleeping to moisturize the air. Humidifiers add some humidity, but generally not enough to make a big difference.
I hope this guide to common upper respiratory tract infections helps you to recognize what kind of medical care you need, if any, and helps you to treat the symptoms of these viral infections at home if that makes sense. Most upper respiratory infections in young, healthy people can be managed at home, without antibiotics but symptoms can last several weeks. And never fear, once you get over this illness, another one is waiting in the wings. If you have concerns about a more serious illness or have an underlying disease or condition, see your doctor.
Fa la la
La la la
La la la
Pin this post and be sure to follow Vermont Mom on Pinterest!













Bookmarking this for all the questions and Googling I will likely (continue to) do in the next few months! It’s already been a rough go, but this article confirmed my decision-making was accurate! Good luck everyone and stay healthy.
Excellent! I’m glad you found it helpful! It was truly a labor of love on my part. I’m hopeful it will help many. Feel free to share with friends and family! Let’s keep people who don’t need a doctor visit home!!
This is great! I feel informed and empowered to make the right choices for my family now and in the years to come. I’m definitely going to get a pulse oximeter.
Excellent! That was the goal! Mission accomplished!
Can I please copy and paste this in my discharge instructions?
Glad you like it! I think that is a question for your medicolegal team! No problem with me to give patients the URL if you feel like it reflects your views on the topic. I’m hoping the college I work for will go in for sending it to our student body( time will tell). But feel free to copy and pats URL onto your private page! I’d really like to do my educational part to keep people home when appropriate!